Rural Provider Self-Care
Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc).
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
Rural Provider Self-Care
Rural Provider PTSD Toolkit

While working with trauma survivors can be very rewarding, you may experience a variety of stress reactions, which overlap.
Click each reaction to learn more.
Click each reaction to learn more.
Burnout
Secondary Traumatic Stress
Compassion Fatigue
Vicarious Traumatization
Burnout
Burnout comprises the emotional and physical exhaustion resulting from both occupational and personal stressors.51-53
Secondary Traumatic Stress
Secondary traumatic stress can occur in those who frequently listen to trauma histories,54,55 with reactions similar to posttraumatic stress disorder (PTSD) symptoms, such as re-experiencing, avoidance, and hyperarousal, anger, low mood, and social isolation.56
Compassion Fatigue
Compassion fatigue is broader than secondary stress and is characterized by the emotional strain experienced when working with individuals coping with traumatic stress.57 It also includes more general symptoms of burnout (e.g., emotional exhaustion).58
Vicarious Traumatization
Vicarious traumatization describes the cognitive, emotional, social, and behavioral changes that may occur while working with traumatized individuals. In particular, views of trust, safety, control, and esteem, may be called into question.59-61
The association between burnout and secondary traumatic stress is high, and they are likely to co-occur among those exposed indirectly to trauma through their work.62 As a rural provider, your self-care may be even more important because of the demands of working in small communities with fewer resources. This lack of resources has been shown to be associated with greater impairment and poorer quality of life in rural Veterans with mental health issues, which may contribute to more burden and greater sense of responsibility in your work.3
How can you be more successful at self-care?
As a provider you are most likely very well aware that there are many different ways to address stress; the key is to learn which strategies work best for you, and proactively put them into practice in a realistic, consistent, and disciplined way.63-73Click an area to learn more.
If work is causing you to feel stressed or burned out, it can sometimes be difficult to identify how big the problem is. If you would like to see how you are doing in comparison with other professionals, there are a number of scales that might be helpful. More information about this and other scales can be found at our Provider Self-Care Toolkit and at ProQOL.org.


If you are experiencing stress reactions, incorporating some self-care strategies may be preventive and helpful in reducing stress.74-78 Generally, successful interventions to address stress reactions combine elements from a number of different categories:
- Social practices such as developing support at home and work, and setting limits can be particularly helpful in rural settings
- Cognitive-philosophical practices such as cognitive restructuring and values clarification and contemplative practices such as mindfulness, daily reflection, and meditation
- Physical practices such as body scanning, exercise, diet, and relaxation practices
While self-care strategies are strongly recommended, workplace support is another important contributor to provider well-being.79 For instance, supervisor support has been shown to be positively related to lower levels of stress reactions, and higher levels of personal growth, accomplishment, and satisfaction.79 Management attention to work rules and structure has also been shown to be a protective factor in burnout.70 Advocating for your colleagues or yourself in regards to workplace support is also a recommended part of any self-care plan.
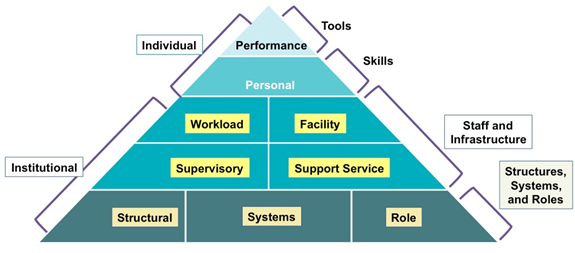
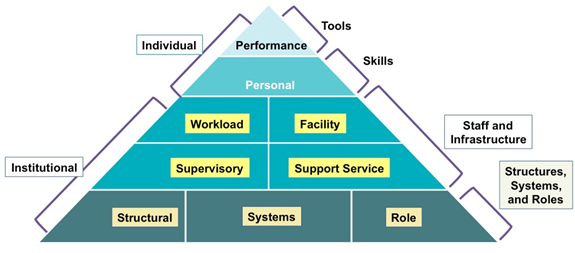
Stress reactions are understandable after a particularly difficult case, or series of cases. Rural providers in particular can also be overloaded with challenging cases based upon their expertise and/or availability of alternative resources. And providers often put the needs of their clients before their own needs. Self-awareness and regular self-monitoring are an important first step to overcoming both internal and external barriers to well-being. The ability to realistically self-assess strengths and vulnerabilities and to be sensitive to signs of difficulties has been shown to be critical to taking constructive action to avoid excessive stress and burnout.80-82 Self-monitoring can help you remain aware of your own possible triggers for distress in personal, professional, and environmental domains.83,84
Strategies
Here are a few specific strategies that may be helpful in increasing self-awareness and well-being in relation to stress a work:Monitor work demands to prevent being overwhelmed
Engage in regular self-reflection and adjustment
Make a list of those strategies that work for you, and keep it close at hand
Get a friend, family member, or colleague involved in checking on you
Make supervision, case conferences, or informal collegial support a priority in your work life
Determine your need for resources, as well as the availability of resources, and make efforts to use them effectively
Be proactive in time management68
Use active cognitive strategies to set appropriate boundaries85
Make efforts to construct a set of practices that enable you to transition out of your work day in a healthy way
Find ways to deal with the issues that may arise around mortality, suffering, loneliness and helplessness
Make time to honor the necessity of working actively to create and maintain a rewarding and meaningful personal life86
If you find that despite the self-care strategies you are actively engaging in, you are still experiencing reactions that interfere with your functioning or persist beyond a month, it may be helpful to seek treatment from a mental health provider. Cognitive behavioral therapy has resulted in positive effects on burnout, and produced greater effects than other types of workplace interventions, such as relaxation and meditation techniques.87
Click to learn more about the resources and support listed below.
Click to learn more about the resources and support listed below.
Self-Care Resources
There are a number of useful mobile apps and online tools to help you manage stress and avoid burnout. Some of the online tools offer self-assessment tracking for you to monitor yourself over time.
This section contains links to provider self-care resources, including web-based learning and tools as well as links to organizations that include helpful materials for providers working with trauma survivors.
Provider Strategies for Coping with Burnout and Secondary Traumatic Stress
This one hour interactive course is designed to provide brief education and dynamic intervention strategies to help address provider stress reactions and improve personal health and resilience. Continuing education credits are offered for this free course.
This one hour interactive course is designed to provide brief education and dynamic intervention strategies to help address provider stress reactions and improve personal health and resilience. Continuing education credits are offered for this free course.
Provider Self-Care Toolkit
This toolkit provides education and resources to help mental health care providers with professional burnout and secondary traumatic stress.
This toolkit provides education and resources to help mental health care providers with professional burnout and secondary traumatic stress.
There are a number of useful mobile apps and online tools to help you manage stress and avoid burnout. Some of the online tools offer self-assessment tracking for you to monitor yourself over time.
Provider Resilience mobile app provides tools and self-assessment monitoring to help health care providers keep themselves productive and emotionally healthy.
Free Provider Resilience download from: Google Play (Android) and iTunes (iOS)
and iTunes (iOS)  .
.
Free Provider Resilience download from: Google Play (Android)
 and iTunes (iOS)
and iTunes (iOS)  .
.
PTSD Coach mobile app offers self-help strategies to manage PTSD or secondary stress symptoms and quick access to support resources.
PTSD Coach Online can help anyone with stress symptoms work in a more in-depth way with "big picture" issues - like understanding your values and goals, or problem solving. Inspired by the PTSD Coach mobile app, PTSD Coach Online is used on a computer, so it is able to incorporate video content and tools that involve writing.
Moving Forward online course includes tools to teach problem solving skills to overcome obstacles and deal with stress. Moving Forward is especially helpful in managing challenges such as: balancing school and family life, financial difficulties, relationship problems, difficult career decisions, and coping with physical injuries.























