Engaging Rural Patients in Psychotherapy
Many barriers to psychotherapy for PTSD are the same for rural and urban Veterans. These include logistical barriers, such as appointment scheduling conflicts, inability to take time off work, and lack of childcare. Attitudinal barriers such as the belief that treatment is not effective, mistrust of therapists, lack of self-efficacy and poor motivation also affect engagement in psychotherapy. However, many barriers facing Veterans are greater for those living in rural areas compared to those living in urban areas including travel time, lack of reliable transportation options, stoicism, self-reliance, stigma, and lack of treatment anonymity. Multiple barriers can compound to create an unsurmountable obstacle to attending weekly appointments for psychotherapy. As a result, rural Veterans are significantly less likely than urban Veterans to initiate psychotherapy, and are significantly less likely to engage in psychotherapy and receive a therapeutic dose.27
Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc).
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
VA »
Health Care »
PTSD: National Center for PTSD
» Providers
»
Engaging Rural Patients in Psychotherapy
PTSD: National Center for PTSD
Engaging Rural Patients in Psychotherapy
Rural Provider PTSD Toolkit
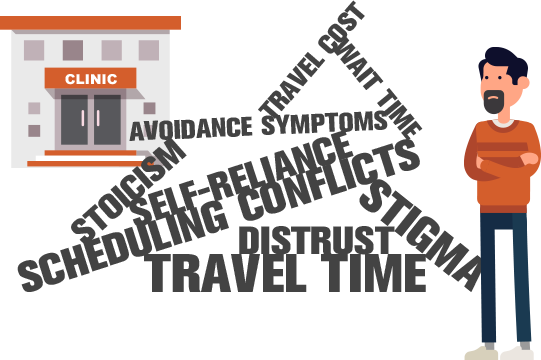
Many rural Veterans live in tight knit communities where they are actively involved in each other's lives. This can raise the apprehension about treatment anonymity and further compound concerns about stigma and discrimination (e.g., job loss). Rural culture also places a high value on self-reliance and stoicism, characteristics that are further reinforced during military service. Health care organizations like VA should work with leaders in rural communities - such as clergy - to address these issues in order to encourage and normalize help seeking among Veterans.28,29
Involving Family
Because family members are often the ones in the best position to detect problems and motivate help seeking, providers can use tools aimed at helping family members encourage loved ones to engage in effective PTSD treatment.30 Resources for this include:Use of Technology
The use of televideo technologies can help mitigate many of the logistical barriers facing rural Veterans. Offering interactive video appointments at VA Community Based Outpatient Clinics reduces travel times and minimizes the time needed to take off from work. To learn more visit Optimizing Rural Care.Utilizing Local Vet Centers
Vet Centers provide readjustment counseling to eligible Veterans, Service members, and their families to help make a successful transition from military to civilian life. Learn more about the Vet Center Program.Collaborative Care
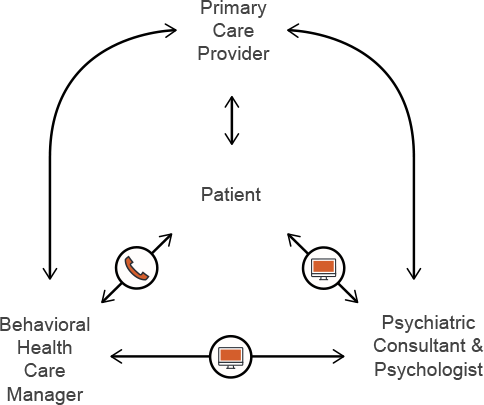
Collaborative care is one approach to promoting engagement in psychotherapy that has been proven to be effective and is now being more widely implemented at VA.31 The cornerstone of the collaborative care model is the care manager who conducts telephone outreach to PTSD patients and uses problem solving, motivational interviewing and shared decision making techniques to activate and engage patients in care.The care manager works closely with telepsychologists and telepsychiatrists to ensure continuity of care, promote adherence to treatment and minimize missed opportunities like no-shows. For psychotherapies with homework, care managers can also help patients practice skills and in vivo exposure exercises. For providers trying to mimic this model, treatment mobile companion applications like CPT Coach and PE Coach also provide reminders for between-session homework and appointments.
Perhaps most importantly, care managers or other providers will gain the trust of rural Veterans over time. This becomes a critical connection to engage the Veteran in high quality treatment.
Collaborative Care Model